Abstract
Salivary cortisol dysrhythmias have been reported in some, but not all studies assessing hypothalamic–pituitary–adrenal (HPA) axis function in Huntington’s disease (HD). These differences are presumed to be due to environmental influences on temporal salivary cortisol measurement. Further exploration of HPA-axis function using a more stable and longer-term measure, such as hair cortisol, is needed to confirm earlier findings. This study aimed to evaluate hair and salivary cortisol concentrations and their associations with clinical and lifestyle outcomes in individuals with premanifest HD (n = 26) compared to healthy controls (n = 14). Participants provided saliva and hair samples and data were collected on clinical disease outcomes, mood, cognition, physical activity, cognitive reserve, sleep quality and social network size to investigate relationships between clinical and lifestyle outcomes and cortisol concentrations. Hair and salivary cortisol concentrations did not significantly differ between the premanifest HD and control groups. No significant associations were observed between hair or salivary cortisol concentrations and cognitive, mood or lifestyle outcomes. However, hair cortisol concentrations were significantly associated with disease outcomes in individuals with premanifest HD. Significant associations between hair cortisol concentrations and measures of disease burden and onset may suggest a potential disease marker and should be explored longitudinally in a larger sample of individuals with HD.
Similar content being viewed by others
Introduction
Hypothalamic–pituitary–adrenal (HPA) axis dysfunction has been suggested to be a key pathological feature and contributor to cognitive, mood and sleep disturbances in individuals with Huntington’s disease (HD)1,2. Studies in animal models and in individuals with HD have nevertheless yielded inconsistent findings, with some but not all investigations reporting acute cortisol dysrhythmias3,4,5.
Early investigations noted a significant elevation in cortisol levels in individuals with manifest HD compared to healthy age and sex matched controls6,7,8. However, more recent studies have been unable to replicate these earlier findings, consistently reporting no differences between individuals with HD and healthy controls. These inconsistent findings have been attributed to differences in sampling methods, as well as a failure to control environmental factors known to influence cortisol release.
To date most investigations have analysed cortisol release from collected blood, urine and saliva samples6,7,8. Two of the existing studies have examined the cortisol awakening response (CAR)6,7, which refers to the sharp increase in cortisol secretion that occurs within the first 30–45 min following awakening in the morning9. This biological phenomenon has been reported to display a consistent pattern in adults and exhibits good intra-individual stability across two days, particularly when total morning cortisol output is examined (area under the curve, AUC)9,10,11. While valid and well-established, these methodological approaches only provide information on short-lived stress, indicated by temporal cortisol release (< 24 h). Furthermore, while informative from a situational context, it is of utmost importance to evaluate longer-term or sustained stress, indicated by cumulative cortisol release, particularly considering the potential impact on cognitive, mood and sleep outcomes5,8,12, which are all negatively impacted in HD13,14,15. It is therefore crucial to identify and evaluate the sensitivity of methodological approaches aimed at examining longer-term stress and associated cumulative cortisol release.
Recent studies in healthy and neurodegenerative populations indicate that hair is a useful biological sample for the analysis of longer-term, cumulative cortisol release. In a recent investigation, Pereira et al.16 noted significantly higher hair cortisol concentrations in individuals with multiple sclerosis compared to healthy controls. Another investigation by Assayag et al.17 reported larger legion volumes and poorer cognitive performance in stroke victims with higher hair cortisol concentrations. Despite these positive findings, the utility of hair as a longer-term measure of cumulative cortisol release has not been investigated in individuals living with HD.
The primary aim of this investigation was to examine differences in hair and salivary cortisol concentrations between individuals with HD and healthy age and sex matched controls. Secondary aims of this investigation included: (1) examination of the environmental factors that significantly influence hair and salivary cortisol concentrations and (2) examination of associations between hair or salivary cortisol concentrations and cognitive and mood outcomes.
Materials and methods
Study design
The aim of this cross-sectional study was to compare hair and salivary cortisol concentrations between individuals with premanifest HD and healthy controls and to examine the relationships between hair or salivary cortisol concentrations and environmental, cognitive and mood measures in individuals with premanifest HD and healthy controls.
Study approval and patient consent
The study was carried out in accordance with the Declaration of Helsinki and was approved by the North Metropolitan Area Mental Health Service (2009_16), Edith Cowan University (13145) and Monash University (CF15/117-2015000058) Human Research Ethics Committees. All participants provided written informed consent prior to undertaking study assessments.
Participants
Twenty-six individuals with premanifest HD and 14 healthy controls participated in the study. Participants were recruited in Perth and Melbourne through the Enroll-HD study database, existing study databases, clinicians and HD community organisations (premanifest HD) and via radio and newspaper advertisement (healthy controls). Inclusion criteria for individuals with premanifest HD were as follows: (1) a cytosine-adenine-guanine (CAG) repeat length of > 39; (2) a Unified Huntington’s Disease Rating Scale (UHDRS) Diagnostic Confidence Level (DCL) of ≤ 2; and (3) a UHDRS Total Motor Score (UHDRS-TMS) of < 5 for presymptomatic or > 5 for prodromal HD18. Exclusion criteria for both groups were as follows: (1) concomitant neurological, cardiovascular, musculoskeletal, endocrine or metabolic disorders, (2) shift work, (3) recent or ongoing substance abuse, (4) current smoker, and (5) the inability to understand written and verbal English.
Study procedures
Participants collected saliva samples on two consecutive mornings. Hair samples (collected by D.B) and cognitive measures (collected by T.C) were obtained from participants on one of the two saliva sampling days. Information regarding mood state and lifestyle activities was collected via self-report questionnaires during week of cortisol sampling. To maintain consistency in sampling and for pragmatic reasons, participants were asked to provide saliva samples on either two consecutive workdays or two consecutive non-workdays, but not a mix of both, with non-workdays suggested. The UHDRS-TMS and DCL assessments were performed by a qualified clinician within four weeks of collection of other study data. CAG repeat length was provided by participants and other disease characteristics, such as estimated age at onset, estimated years to onset, disease burden score and CAG-age product score (CAPs) were calculated using previously established methods19,20,21. Sociodemographic characteristics were collected via a questionnaire. Body mass index (BMI) was calculated by dividing the participant’s weight (in kg) by their height squared (m2), with dual energy x-ray absorptiometry (DXA; Hologic Discovery A, Waltham, MA, USA) and wall mounted stadiometer (Model 222, Seca, Hamburg, DE) used to collect weight and height, respectively.
Cortisol measures
Hair cortisol
Hair samples were cut from the vertex posterior area of the head, as close to the scalp as possible. The first 3 cm of hair from the scalp end was used to assess cortisol concentrations over the previous three months, based on the assumption that hair grows at a rate of approximately 1 cm per month22. The hair washing and cortisol extraction procedures were carried out in line with a pre-existing protocol23. Briefly, hair was washed twice in isopropanol and then left to air dry. The hair was weighed and transferred to 2 mL bead beating tubes containing 2.8 mm ceramic beads (Qiagen, Germany). Hair samples were ground using the Powerlyzer 24 homogeniser and then methanol was added to the samples and incubated overnight (16 h) at room temperature for steroid extraction. Methanol was completely evaporated using a Speedvac Savant concentrator and dry samples were then eluted in 200 µL of phosphate buffered saline. Cortisol concentrations were determined using salivary cortisol enzyme-linked immunosorbent assay (ELISA) kits (IBL-International, Hamburg, Germany), according to the manufacturer’s instructions. The intra-assay coefficients of variation (CV) were below 5% and the inter-assay CV was 13.5%. The functional sensitivity of the assay was reported to be 0.138 nmol/L.
Salivary cortisol
Saliva samples were collected by participants in their own homes on two consecutive days. Participants were instructed on how to collect saliva samples during a face-to-face meeting with a study investigator and were provided with detailed instructions on how and when to collect saliva samples. Participants were instructed to passively drool into four separate polypropylene collection tubes (SSI Bio) at four time points in the morning at 15, 30, 45 and 60 min following awakening for morning cortisol analysis7. To avoid contamination of samples, participants were instructed to refrain from consuming alcohol 12 h prior and to avoid eating, drinking (with the exception of water) and brushing their teeth within the sampling time frame7. Participants were provided with a diary to note down their time of awakening and when saliva samples were taken and to confirm that they had not consumed anything except water and had refrained from smoking, brushing their teeth and exercising during the saliva sampling period. Participants stored saliva samples in their freezer until collection by a study investigator on the second day of sampling. Saliva samples were then stored at − 80 °C in the laboratory until analysis in duplicate using salivary cortisol ELISA kits (Salimetrics, USA) according to the manufacturer’s instructions. All intra-assay CVs were below 10% and the inter-assay CV was 7.3%. The functional sensitivity of the assay was reported to be 0.773 nmol/L. The CAR and area under the curve with respect to ground (AUCG) were calculated using the methods described by van Duijn et al.7. Briefly, CAR was calculated by averaging the cortisol concentrations between the 45- and 60-min time points and then subtracting the cortisol concentration of the first time point. AUCG was calculated using the trapezoid rule to determine total morning cortisol release for each day. The variation in cortisol AUCG values between sampling days was below 13% for both groups. Both the CAR and AUCG values were averaged across the two sampling days7.
Affective measures
The 14-item Perceived Stress Scale was used to measure stress over the previous month. The Hospital Anxiety and Depression Scale (HADS) was used to measure anxiety and depression symptomatology. The HADS is a 14-item questionnaire, with 7 items each relating to symptoms of anxiety and depression.
Cognitive measures
The Hopkins Verbal Learning Test-Revised (HVLT-R) was used to evaluate verbal learning and memory. The One Touch Stockings (OTS) assessment was used to evaluate planning and problem solving. The Trail Making Test (TMT; Parts A and B) was used to examine attention and cognitive flexibility. The Symbol Digit Modalities Test (SDMT) was used to assess processing speed.
Lifestyle measures
Lifestyle measures included self-report physical activity, cognitive reserve, social network, sleep quality, smoking and alcohol consumption questionnaires. Physical activity was evaluated using the Minnesota Leisure Time Physical Activity Questionnaire. Cognitive reserve was calculated using values obtained from Cognitive Activity Scale, National Adult Reading Test, occupation and education status. Smoking status (packets per week) and alcohol consumption (standard drinks per week) were evaluated using a custom questionnaire. Social network size and diversity was evaluated using the Social Network Index. Sleep quality was measured using the Pittsburgh Sleep Quality Index. These measures were purposefully selected as they have been shown to be associated with measures of disease progression in HD24,25 as well as cortisol regulation in the elderly and other clinical populations26,27.
Statistical analysis
Based on sample size estimations, 29 participants were required per group (α = 0.05, 1 − β = 0.8)28. However, as this study was ancillary to another study, recruitment was limited to the participant pool of the parent study, as well as other factors such as hair length, pigment loss and hair dying.
Rstudio (RStudio Team 2015) Version 1.2.5033 for Macintosh was used for all statistical analyses. Specific statistical packages within R were used where required and if not stated are available within the base R functionality. Summary analyses of demographic, cognition and environmental variables provided means/counts and standard deviations/percentages stratified by disease classification (premanifest HD versus healthy controls. T-tests (age, perceived stress scale) and chi-squared tests (site, sex) were used to assess the differences between demographic measures.
Data normality was assessed using Shapiro–Wilk tests and analyses were undertaken accordingly. Hair cortisol and salivary cortisol data were not normally distributed. All other data fit the normal distribution. Analyses of covariance (ANCOVA), controlling for age and sex, were performed to assess differences in hair and salivary cortisol concentrations between individuals with premanifest HD and healthy controls. Associations between clinical classification, HD characteristics, cognition and environment, and cortisol levels (both hair and salivary) were investigated. Spearman’s partial correlations were used to assess relationships between variables, with age, sex and disease burden included as covariates, where appropriate.
Results
Demographic and clinical characteristics
Participants ranged in age from 22 to 70 (premanifest HD) and 21 to 58 (healthy controls). BMI ranged between 20.8 to 33.4 (premanifest HD) and 19.1 to 28.7 (healthy controls). Healthy controls exhibited significantly higher stress levels, as indicated by the Perceived Stress Scale, than individuals with premanifest HD (Table 1). No other differences were observed between groups across demographic and clinical characteristics.
Between-group comparisons of hair and salivary cortisol concentrations
No differences were observed in cumulative hair cortisol or temporal salivary cortisol concentrations between premanifest HD and healthy control groups (Table 2).
Between-group comparisons of cognitive and lifestyle outcomes
Individuals with premanifest HD performed significantly worse than healthy controls on measures of verbal learning and memory (HVLT-R), planning and problem solving (OTS), attention (TMT-A), cognitive flexibility (TMT-B) and processing speed (SDMT; Table 2). No other significant differences were observed for cognitive or lifestyle measures between the groups.
Correlations between hair and salivary cortisol concentrations and cognitive and lifestyle measures
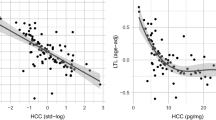
Significant associations were noted between hair cortisol concentrations and clinical disease outcomes in the premanifest HD group (Table 3). In particular, these associations were observed for disease burden score and the estimated number of years to disease onset. No other significant associations were observed between cumulative hair or temporal salivary cortisol concentrations and clinical, cognitive or lifestyle measures in the premanifest HD or healthy control groups.
Discussion
Abnormalities in cortisol release have been reported previously in individuals with HD and have been suggested to be an indicator of hypothalamic–pituitary–adrenal (HPA) axis pathology29,30. However, these studies used salivary cortisol as the principal output, which is prone to temporal changes in response to environmental and psychological stimuli. Accumulative cortisol in hair has been proposed as a measure of longer-term or sustained stress. Here, we examined, for the first time, hair cortisol concentrations in individuals with premanifest HD in comparison to healthy controls. Furthermore, we assessed the relationships between cumulative cortisol in hair and shorter-term temporal salivary cortisol and clinical, cognitive and lifestyle measures in individuals with premanifest HD. We report no significant differences between groups in longer-term or sustained stress, as indicated by cumulative hair cortisol concentrations. Furthermore, we note no significant associations between hair or salivary cortisol concentrations and environmental and clinical outcomes.
Previous studies have noted significant differences in saliva cortisol concentrations between individuals with HD and healthy controls7,8. We were unable to replicate these earlier findings in our cohort. In particular, we found no differences in hair and salivary cortisol concentrations between individuals with premanifest HD and healthy controls. This was unexpected. Given that regulation of the CAR, and cortisol release in general, involves the hippocampus, amygdala, prefrontal cortex and suprachiasmatic nucleus31,32 and considering the known pathological changes to these structures to varying extents in HD29,30,33,34, it was anticipated that differences between hair and salivary cortisol metrics would be observed. The reason for the discrepancy in findings is not known, however it is noteworthy that, contrary to previous reports7,35, stress levels were significantly lower in the premanifest HD group than in healthy controls. Interestingly, cumulative hair cortisol concentrations were found to be associated with disease burden score and the estimated number of years to disease onset, initially suggesting that it may be a potential candidate for a biological marker of disease progression. However, considering no differences were observed in cumulative hair cortisol concentrations between the groups, this may represent a coincidental finding. In addition, CAR metrics did not appear to be a sensitive marker in this group, despite earlier findings7. Nevertheless, both cortisol measurements should be evaluated longitudinally to definitively assess whether they change over time as the disease progresses.
Associations between clinical outcomes, including mood and cognitive outcomes, and temporal salivary cortisol release have been reported previously in HD5,8. Shirbin et al. reported associations between short-term salivary cortisol release and depressive symptomology and performance on verbal learning and memory tasks5,8. These earlier findings were not reflected in the present study. In particular, no associations were observed between hair or salivary cortisol release and cognitive and mood outcomes in individuals with HD. It is possible that these relationships do not arise until late in the disease course, where symptoms of the disease progressively emerge.
Preclinical studies have previously documented positive effects of environmental enrichment on HPA-axis structures, including the adrenal glands, which are involved in the regulation of glucocorticoids36. Studies in older adults and other clinical populations, including schizophrenia, have additionally reported a negative effect of unhealthy lifestyle behaviours, such as physical inactivity and social isolation on cortisol regulation27,37. It was therefore hypothesised that lifestyle factors, particularly physical activity, cognitive reserve and social network size would be negatively associated with cortisol levels such that greater physical activity, cognitive reserve and social network size would be associated with lower cortisol levels. Our findings did not support this hypothesis, with no associations observed between hair or salivary cortisol levels and any of the lifestyle factors. However, it should be noted that this study adopted a cross-sectional design, it is possible that associations between cortisol and lifestyle outcomes may arise over time, particularly as the disease advances.
Several limitations need to be considered when interpreting our findings. First, this was a cross-sectional investigation of associations between cortisol concentrations and clinical and environmental outcomes, subsequently causation cannot be determined. Second, this study had a relatively small sample of participants with premanifest HD and healthy age and sex matched controls. Therefore, it is not known whether associations between cortisol and clinical and environmental outcomes manifest later in the disease course, which has been described, albeit only in a few studies previously. It is important to note that this study consisted predominantly of female participants. While this was not intended, this may bias the results, particularly as females may have different cortisol rhythms to males and these are influenced by menstrual events. It is also noteworthy that the timing of saliva sampling was self-reported, which can be influenced by responder and recall bias. This bias might be overcome in the future by using tubes with timing caps, which has been suggested by Stalder et al.38. Finally, cortisol has been shown to be influenced by seasonal changes. Participants in this study were sampled in Australia only (Melbourne and Perth) during spring, when there is progressively greater sunlight and better weather conditions. This may be in contrast to previous studies that may have taken cortisol samples in winter months, when there is less sunlight and poorer weather conditions. Future studies are needed to evaluate changes in hair and salivary cortisol, and the potential associations with clinical and environmental outcomes, longitudinally.
Despite the abovementioned limitations, it is important to note that this is the first study to investigate longer-term or sustained stress as indicated by cumulative cortisol concentrations in hair in individuals with premanifest HD. Furthermore, this is the first study to evaluate associations between longer-term or sustained stress, indicated by cumulative cortisol release, and shorter-lived stress, indicated by temporal cortisol release, and environmental outcomes in individuals with premanifest HD. In contrast to previous findings, we observed no differences in hair or salivary cortisol concentrations between individuals with premanifest HD or healthy controls. In addition, we found no associations between cortisol concentrations and mood, cognitive and environmental outcomes. Small to moderate associations were found between hair cortisol concentrations and measures of disease burden, however, as no differences were observed between groups this is likely a spurious finding. Nevertheless, this latter finding provides impetus for further investigation of longer-term or sustained cortisol and associations with clinical and environmental outcomes longitudinally.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Petersén, Å. & Björkqvist, M. Hypothalamic–endocrine aspects in Huntington’s disease. Eur. J. Neurosci. 24, 961–967. https://doi.org/10.1111/j.1460-9568.2006.04985.x (2006).
Bartlett, D. M. et al. Neuroendocrine and neurotrophic signaling in Huntington’s disease: implications for pathogenic mechanisms and treatment strategies. Neurosci. Biobehav. Rev. 71, 444–454. https://doi.org/10.1016/j.neubiorev.2016.09.006 (2016).
Aziz, N. A. et al. Increased hypothalamic–pituitary–adrenal axis activity in Huntington’s disease. J. Clin. Endocrinol. Metab. 94, 1223–1228. https://doi.org/10.1210/jc.2008-2543 (2009).
Saleh, N. et al. Neuroendocrine disturbances in Huntington’s disease. PLoS ONE 4, e4962 (2009).
Shirbin, C. A. et al. The relationship between cortisol and verbal memory in the early stages of Huntington’s disease. J. Neurol. 260, 891–902 (2013).
Hubers, A. A. et al. Hypothalamic–pituitary–adrenal axis functioning in Huntington’s disease and its association with depressive symptoms and suicidality. J. Neuroendocrinol. 27, 234–244. https://doi.org/10.1111/jne.12255 (2015).
van Duijn, E. et al. Hypothalamic–pituitary–adrenal axis functioning in Huntington’s disease mutation carriers compared with mutation-negative first-degree controls. Brain Res. Bull. 83, 232–237. https://doi.org/10.1016/j.brainresbull.2010.08.006 (2010).
Shirbin, C. A. et al. Cortisol and depression in pre-diagnosed and early stage Huntington’s disease. Psychoneuroendocrinology 38, 2439–2447 (2013).
Pruessner, J. C. et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 61, 2539–2549. https://doi.org/10.1016/S0024-3205(97)01008-4 (1997).
Hucklebridge, F., Hussain, T., Evans, P. & Clow, A. The diurnal patterns of the adrenal steroids cortisol and dehydroepiandrosterone (DHEA) in relation to awakening. Psychoneuroendocrinology 30, 51–57 (2005).
Wust, S. et al. The cortisol awakening response-normal values and confounds. Noise Health 2, 79 (2000).
Vgontzas, A. N. et al. Impaired nighttime sleep in healthy old versus young adults is associated with elevated plasma interleukin-6 and cortisol levels: physiologic and therapeutic implications. J. Clin. Endocrinol. Metab. 88, 2087–2095. https://doi.org/10.1210/jc.2002-021176 (2003).
Herzog-Krzywoszanska, R. & Krzywoszanski, L. Sleep disorders in Huntington’s disease. Front. Psychiatry 10, 221 (2019).
Stout, J. C. et al. Evaluation of longitudinal 12 and 24 month cognitive outcomes in premanifest and early Huntington’s disease. J. Neurol. Neurosurg. Psychiatry 83, 687–694. https://doi.org/10.1136/jnnp-2011-301940 (2012).
Tabrizi, S. J. et al. Biological and clinical manifestations of Huntington’s disease in the longitudinal TRACK-HD study: cross-sectional analysis of baseline data. Lancet Neurol. 8, 791–801. https://doi.org/10.1016/s1474-4422(09)70170-x (2009).
Pereira, G. M. et al. Hair cortisol concentration, cognitive, behavioral, and motor impairment in multiple sclerosis. J. Neural Transm. 126, 1145–1154 (2019).
Assayag, E. B. et al. High hair cortisol concentrations predict worse cognitive outcome after stroke: results from the TABASCO prospective cohort study. Psychoneuroendocrinology 82, 133–139 (2017).
Ross, C. A. et al. Movement disorder society task force viewpoint: Huntington’s disease diagnostic categories. Mov. Disord. 6, 541–546 (2019).
Zhang, Y. et al. Indexing disease progression at study entry with individuals at-risk for Huntington disease. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. Off. Publ. Int. Soc. Psychiatr. Genet. 156b, 751–763. https://doi.org/10.1002/ajmg.b.31232 (2011).
Penney, J. B. J., Vonsattel, J. P., MacDonald, M. E., Gusella, J. F. & Myers, R. H. CAG repeat number governs the development rate of pathology in Huntington’s disease. Ann. Neurol. 41, 689–692. https://doi.org/10.1002/ana.410410521 (1997).
Langbehn, D. R., Hayden, M. R. & Paulsen, J. S. CAG-repeat length and the age of onset in Huntington disease (HD): a review and validation study of statistical approaches. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 153, 397–408 (2010).
Stalder, T. & Kirschbaum, C. Analysis of cortisol in hair-state of the art and future directions. Brain Behav. Immun. 26, 1019–1029. https://doi.org/10.1016/j.bbi.2012.02.002 (2012).
Meyer, J., Novak, M., Hamel, A. & Rosenberg, K. Extraction and analysis of cortisol from human and monkey hair. J. Vis. Exp. https://doi.org/10.3791/50882 (2014).
Bonner-Jackson, A. et al. Cognitive reserve and brain reserve in prodromal Huntington’s disease. J. Int. Neuropsychol. Soc. JINS 19, 739–750. https://doi.org/10.1017/s1355617713000507 (2013).
Trembath, M. K. et al. A retrospective study of the impact of lifestyle on age at onset of Huntington disease. Mov. Disord. 25, 1444–1450. https://doi.org/10.1002/mds.23108 (2010).
Feller, S. et al. Predictors of hair cortisol concentrations in older adults. Psychoneuroendocrinology 39, 132–140 (2014).
Ho, R. T. H. et al. Associations between diurnal cortisol patterns and lifestyle factors, psychotic symptoms, and neurological deficits: a longitudinal study on patients with chronic schizophrenia. J. Psychiatr. Res. 81, 16–22 (2016).
Costa, C. M. et al. Levels of cortisol and neurotrophic factor brain-derived in Parkinson’s disease. Neurosci. Lett. 708, 134359. https://doi.org/10.1016/j.neulet.2019.134359 (2019).
Bartlett, D. M. et al. Investigating the relationships between hypothalamic volume and measures of circadian rhythm and habitual sleep in premanifest Huntington’s disease. Neurobiol. Sleep Circ. Rhythms 6, 1–8 (2019).
Kassubek, J. et al. Topography of cerebral atrophy in early Huntington’s disease: a voxel based morphometric MRI study. J. Neurol. Neurosurg. Psychiatry 75, 213–220 (2004).
Herman, J. P. & Cullinan, W. E. Neurocircuitry of stress: central control of the hypothalamo–pituitary–adrenocortical axis. Trends Neurosci. 20, 78–84 (1997).
Herman, J. P., Ostrander, M. M., Mueller, N. K. & Figueiredo, H. Limbic system mechanisms of stress regulation: hypothalamo–pituitary–adrenocortical axis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 29, 1201–1213 (2005).
Politis, M. et al. Hypothalamic involvement in Huntington’s disease: an in vivo PET study. Brain 131, 2860–2869. https://doi.org/10.1093/brain/awn244 (2008).
Soneson, C. et al. Early changes in the hypothalamic region in prodromal Huntington disease revealed by MRI analysis. Neurobiol. Dis. 40, 531–543. https://doi.org/10.1016/j.nbd.2010.07.013 (2010).
Downing, N. et al. Perceived stress in prodromal Huntington disease. Psychol. Health 27, 196–209. https://doi.org/10.1080/08870446.2010.529141 (2011).
Du, X. et al. Environmental enrichment rescues female-specific hyperactivity of the hypothalamic–pituitary–adrenal axis in a model of Huntington’s disease. Transl. Psychiatry 2, e133. https://doi.org/10.1038/tp.2012.58 (2012).
Iob, E., Kirschbaum, C. & Steptoe, A. Positive and negative social support and HPA-axis hyperactivity: evidence from glucocorticoids in human hair. Psychoneuroendocrinology 96, 100–108 (2018).
Stalder, T. et al. Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology 63, 414–432 (2016).
Acknowledgements
The authors would like to thank the participants for their time and contribution to this study. Authors would also like to thank Huntington’s Western Australia for their invaluable assistance throughout the project. Finally, authors would like to acknowledge Prof Nellie Georgiou-Karistianis, Dr Catarina Kordsachia, Ms Linda Hoult, Dr Pauline Zaenker, Mr Tim Rankin and Prof Brian Power for their contributions to the project. This work was supported by Lotterywest (MZ and TC; # 107/20090827).
Author information
Authors and Affiliations
Contributions
T.C., M.Z. and D.M.B. conceptualised the study. T.C., T.P. and D.M.B. wrote the manuscript. D.M.B. and T.C. collected the data. T.P. and S.M.L. analysed the data. All authors contributed to data interpretation and review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cruickshank, T., Porter, T., Laws, S.M. et al. Hair and salivary cortisol and their relationship with lifestyle, mood and cognitive outcomes in premanifest Huntington’s disease. Sci Rep 11, 5464 (2021). https://doi.org/10.1038/s41598-021-84726-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84726-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.